Ailevate Revenue Recovery is an on-prem AI solution for AI-powered denial resolution- automatically correcting coding errors in denied claims without manual work or workflow disruption.

Every year, 15–20% of claims are denied on first submission. Most go unrecovered due to manual rework constraints. Even advanced RCM platforms only alert you to the problem—they don’t fix it.
Ailevate Revenue Recovery uses AI agents to identify and correct coding errors in denied claims – helping you recover more revenue without expanding your billing team.
Ailevate’s AI agents work in the background to identify and correct coding errors in denied claims—reducing manual rework and accelerating revenue recovery.
| Feature | Ailevate Revenue Recovery | Traditional RCM Tools | Outsourced Billing |
|---|---|---|---|
| Denial Recovery | |||
| Operational Costs | |||
| Speed to Revenue | |||
| Scalability |

Integrates with your existing billing system.
AI workforce applies corrective actions based on root cause analysis caused by coding errors from denial claims.
Corrects denial issues and hands off clean claims for your team to resubmit, keeping oversight where it matters.
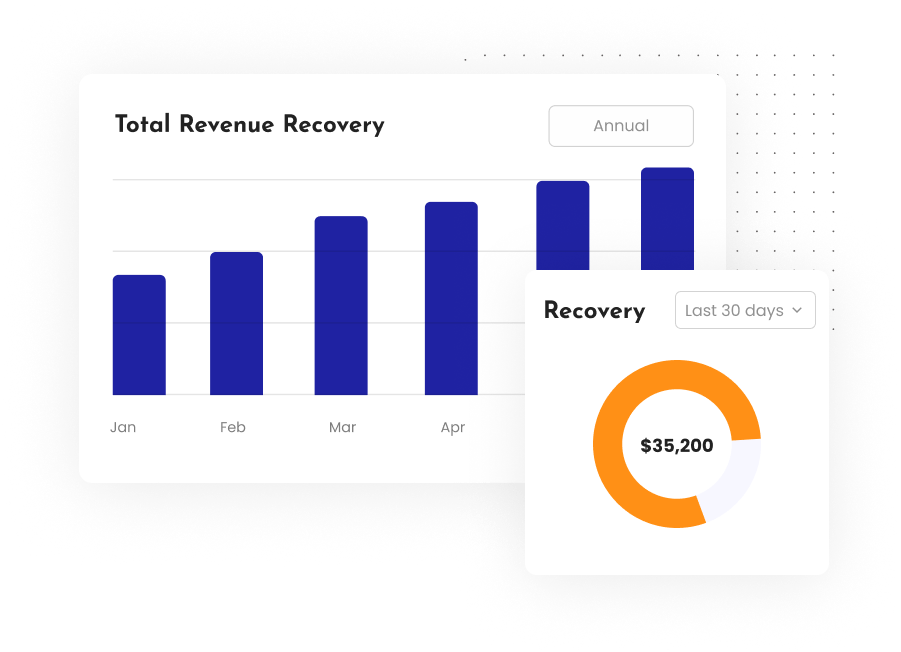
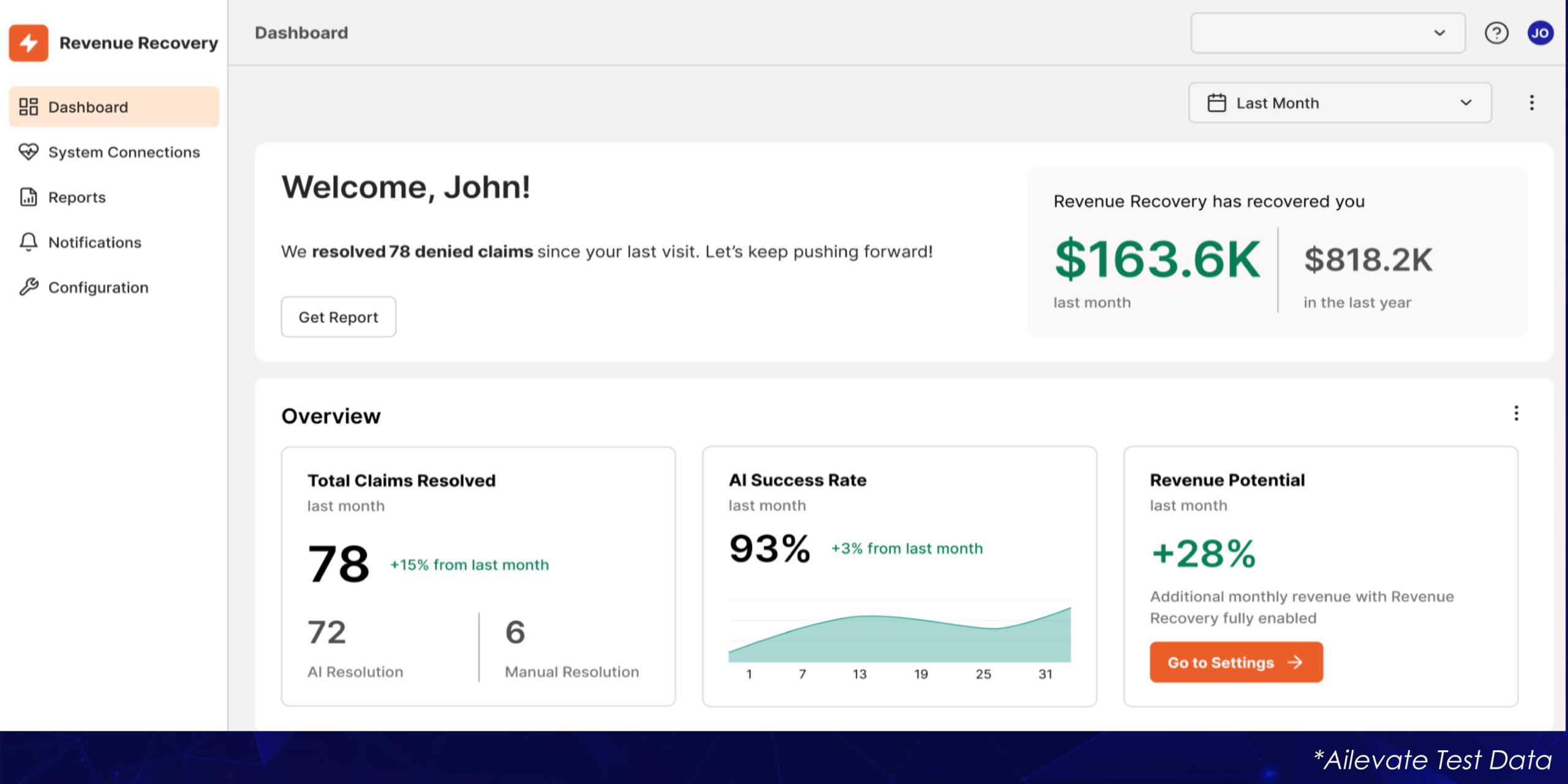
Get a clear dashboard of dollars recovered, denial trends, and preventable risks.
Unlike cloud-based RCM tools, Ailevate runs on-prem, eliminating:
Ailevate keeps all patient data secure in your data center while maximizing ROI.

Turn your denials into dollars—without adding staff or changing workflows.